Abstract

Background: Pulmonary hypertension (PH) in adults with sickle cell disease (SCD) is associated with significant morbidity and early mortality. Venous thromboembolism (VTE) is common in SCD and affects about 25% of SCD adults. Although not generally considered a major cause of PH, chronic thromboembolic pulmonary hypertension (CTEPH) has been noted, and is probably more common than realized in patients with SCD. National guidelines recommend that CTEPH should be excluded in any patient suspected to have PH. Imaging techniques, including ventilation-perfusion (V/Q) scintigraphy, multidetector CT pulmonary angiography (CTPA), high-resolution CT (HRCT), pulmonary digital subtraction angiography (DSA), and magnetic resonance angiography have been used in identifying CTEPH as the cause of PH. Several studies have shown that V/Q scintigraphy is able to distinguish patients with CTEPH from other causes of PH, to the extent that normal V/Q scintigraphy can comfortably rule out CTEPH. However, data on V/Q and associated outcomes on SCD are limited. In this study, we report a retrospective analysis of V/Q scintigraphy findings and CTPA for assessing PH as validated by right heart catherization. We also report associated outcomes of the V/Q findings with prospectively collected data in the adult SCD patients.
Methods: This study was approved by the Institutional Review Board at the National Institutes of Health (NIH), and all subjects provided written informed consent to one or more studies.
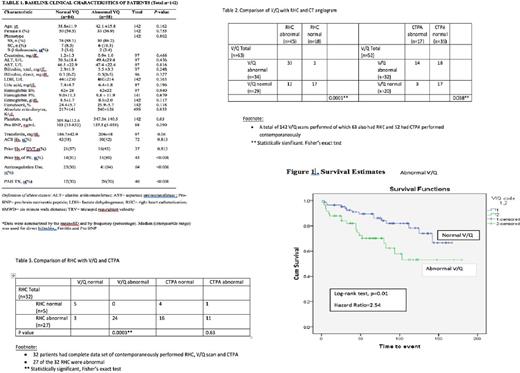
A total of 142 consecutive patients, (83 women, aged 40.1 ± 13.7 years, HbSS 124 (87%) suspected of having PH were prospectively enrolled (Table 1). All patients underwent V/Q scanning, echocardiography (ECHO), six-minute walk testing (6MWT); 52 patients underwent CTPA, and 63 patients had right heart catheterization (RHC) performed. Interpretation of V/Q images was based on the refined Pulmonary Embolism Diagnosis criteria. High-probability and intermediate-probability V/Q scan findings were considered to be positive or abnormal, and very low, low-probability/normal V/Q scan findings were considered negative or normal V/Q.
Results: V/Q scan was abnormal in 58 (40.8%) patients (high probability and intermediate probability in 26 (18.3%), 32 (22.5%), respectively), and was low probability/normal in 84 (59.2%) patients (Table 1). CTPA was positive for PE in 17 (32.7%) patients. Patients with positive CTPA were more likely to have abnormal V/Q [ abnormal V/Q 14 (82.4%) vs. normal V/Q 3(17.6); p=0.032], but in those with negative CTPA (n=35), V/Q was abnormal in 18 (51.4%) (Table 2). RHC confirmed PH (mean pulmonary artery pressure (mPAP) ≥25mmHg) in 45/63 patients, of which 33 (73.3%) had abnormal V/Q compared to 12 (26.6%) with normal V/Q scans, (p=0.0001). Among those with no PH by RHC (n=18), only one patient showed abnormal and 17 normal V/Q (5.6% vs 94.4%, respectively, (p<0.001). Thirty-two patients had a complete dataset of V/Q, CTPA and RHC, and clearly there was greater concordance of results between RHC with V/Q than CTPA (Table 3). Subjects with SCD and abnormal V/Q demonstrated significantly worse hemodynamic severity (mPAP=35.95 ± 9.20 vs.24.8± 12.09 mmHg, p<0.001; right atrial pressure= 9.59± 4.53 vs. 9.59± 4.53mmHg, p<0.001; transpulmonary gradient 21.8 ± 10.4 vs. 12.16± 11mmHg, p=0.001, and pulmonary vascular resistance=238.3 ± 135 vs.120.5 ± 134.9 dynes.s.cm-5, p=0.001 ) and abnormal cardiopulmonary markers of clinical severity compared to those with a normal V/Q group, including higher TRV (3.5±0.6 vs. 3±0.5 m/s, p=0.01) and poor exercise capacity (6MWD 379.7±117.3 vs. 438.8±115.5m, p<0.001). Over a median follow-up of 6 years with a maximum follow-up of 15 years, total of 34 deaths were observed (Fig 1). The all-cause mortality was higher in the abnormal V/Q 19 (56%) group compared to those with normal V/Q 15 (44%) patients (log-rank test, p<0.001, Hazard Ratio=2.54).
Conclusion: Using RHC as the benchmark, our data demonstrates that V/Q scan is superior in detecting CTEPH in adults with SCD. Additionally, abnormal V/Q scan is associated with worse hemodynamics by RHC, poor functional capacity and increased mortality. We recommend frequent use of V/Q in the evaluation of dyspnea in adults with SCD as confirmation of CTEPH has important implications in management.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal